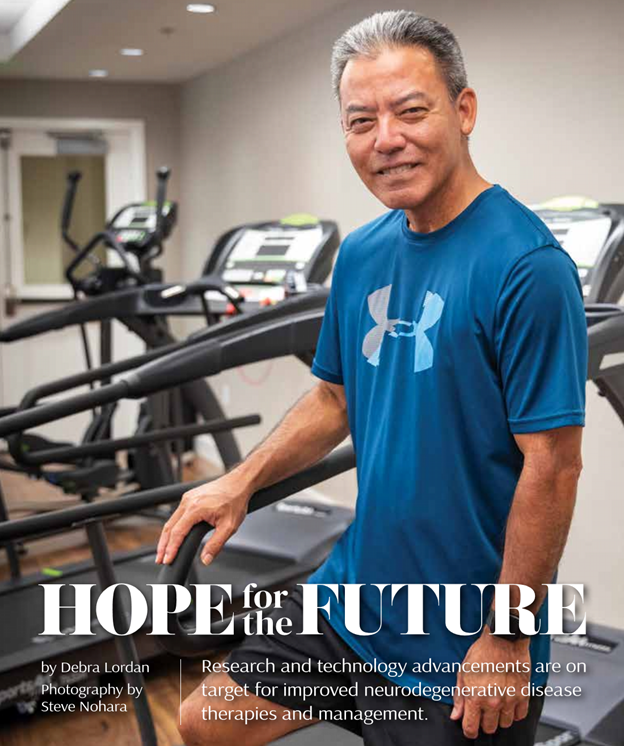
Glen Higa of Kalihi has much in common with Michael J. Fox. Like the “Back to the Future” star, he faces his challenges with gratitude and optimism, focusing on finding meaning in the face of adversity. Like Michael, he emphasizes that challenges don’t define a person—their actions do. He believes in the power of acceptance and the importance of making the best of a difficult situation. Like Michael, he has dedicated himself to making a profound difference in the lives of those affected by a debilitating condition.
In 1998, Michael J. Fox stunned the world by announcing he had been diagnosed with young-onset Parkinson’s disease (PD), also called early-onset Parkinson’s—a degenerative neurological condition. He was diagnosed in 1991 at age 29, but had kept it a secret for seven years.
His memoirs chronicle his Parkinson’s journey and his advocacy work. “Lucky Man,” “Always Looking Up,” “No Time Like the Future” and “A Funny Thing Happened on the Way to the Future” describe what it’s like to be a 30-year-old who has been told he has an 80-year-old’s disease. He shares an inspiring account of his experiences and the lessons he has learned.
Before his diagnosis, the aspiring young actor envisioned a future centered on a flourishing career and family life. PD prompted a paradigm shift, leading him to prioritize the here and now. He established the Michael J. Fox Foundation (MFF) for Parkinson’s Research in 2000, which has become the axis around which his life revolves. The foundation is the driving force and primary focus of his existence and aspirations for the future.
Glen’s Life Transformation
“I was diagnosed seven years ago in 2018 at the age of 48, though looking back, I had developed symptoms over five years before,” says Glen, now 55. “Six months after my diagnosis, I left my longtime career as a sales and marketing executive to focus on my health.”
Glen’s proactive attitude is key to successfully managing PD. “I started working with a personal trainer a year after I was diagnosed and it transformed my life,” says Glen. “I did so well with my exercise therapy that I resumed playing softball.” Since being diagnosed, he has participated in the Los Angeles Dodgers Adult Baseball Camp and continues to play competitive softball.
Ultimately, Glen turned his own therapy into a new career by becoming a personal trainer three years after being diagnosed, working exclusively with people who have Parkinson’s.
What is Parkinson’s Disease?
PD is the fastest growing neurodegenerative disease in the world. Nearly 1 million people in the US and more than 6 million people worldwide are affected. PD occurs when brain cells that make dopamine, a chemical that coordinates movement, stop working or die, according to michaeljfox.org, an informational website Glen recommends highly. This “movement disorder” can cause tremor, slowness, stiffness, and walking and balance problems. Constipation, depression, memory problems and other non-movement symptoms can also surface as symptoms.
PD is a lifelong progressive disease—symptoms slowly worsen over time. But the experience of living with PD is unique to each person. As symptoms and progression vary from person to person, neither you nor your doctor can predict which symptoms you will get, when you will get them or how severe they will be. Even though similarities are observed among individuals with PD as the disease progresses, there is no guarantee you will experience what you see in others.
What is Early-Onset PD?
According to Fox’s website, about 10% to 20% of people with PD experience symptoms before age 50. While treatments are the same for early-onset Parkinson’s disease (EOPD), younger people may experience the disease differently.
People with EOPD may have a longer journey to diagnosis, sometimes seeing multiple doctors and undergoing several tests before reaching a correct conclusion. As with PD diagnosed later in life, EOPD is diagnosed based on a person’s medical history and physical examination.
When younger people and their clinicians are not expecting PD, the diagnosis may be missed or delayed. It’s not uncommon for arm or shoulder stiffness to be attributed to arthritis or even a sports injury before PD is eventually diagnosed. Scientists are working to understand the causes of early-onset Parkinson’s.
What is Wrong With Me?
Glen describes his initial suspicions and symptoms that led him to seek medical intervention.
“My girlfriend and I would walk daily around Diamond Head after work and she noticed I stopped swinging my arms and that I shuffled my feet while walking,” says Glen. “My legs started to feel heavy. Soon after, I started experiencing shoulder and neck stiffness and a tremor in my left hand. But an official diagnosis wouldn’t come until more than two years later.”
“My first thought after the EOPD diagnosis was a sense of relief,” says Glen. “Honestly! I didn’t know what was going on in my head—if I had a stroke, tumor, aneurysm or something else!
“I was seeing a physical therapist who told me I was showing symptoms of Parkinson’s, but I guess I didn’t take his comments seriously at first. But when my neurologist told me I could still live a good life with Parkinson’s, she eased my mind and I was ready to do what I had to do to achieve that good life.”
“Most of my friends, family and coworkers noticed something was not right before I was diagnosed,” Glen adds. “So I told everyone about it and didn’t try to hide it from anyone. Almost everyone reacted positively and said they were ready to help when needed. Being supportive and showing empathy— but not sympathy— go a
long way.”
‘You can live your best life.’
Glen first became involved with Hawai‘i Parkinson’s Association (HPA) in 2019, serving in a marketing and administrative support role. HPA, established in 1996, is a nonprofit volunteer group comprised of people with PD, caregivers, family members, healthcare professionals, educators and leaders in the business community. HPA aims to positively impact the lives of people affected by Parkinson’s through support, programs, education and other valuable services.
“The reason why I ran for president was to show those diagnosed with EOPD and those who are living with PD to not be afraid of the condition,” says Glen. “I wanted to spread the message that you can live your best life with PD and dispel the myths believed by people who are not familiar with Parkinson’s. It is not terminal. I also want to show everyone that people with Parkinson’s are abled and not disabled. While there is no cure and it is not a fun existence, you can still live a good life and do things that others do.”
Glen’s focus as the current president is to continue engaging the Parkinson’s community through his position as a “local boy” with Parkinson’s and encourage others there is HOPE—Healthy Overcomes Parkinson’s Everyday.
“As president of HPA, I focus on reducing the perceived stigma of PD,” says Glen. “While there is more awareness and people are more open about their diagnosis, there are still too many unwilling to disclose their condition out of fear, shame or guilt… Especially difficult to reach groups are those with EOPD, Asians (particularly males), Native Hawaiians, Polynesians and those who are economically disadvantaged.”
As an EOPD patient and HPA president, Glen offers recommendations for those who are diagnosed with PD.
“The first step is to join a support group,” he says. “We consider that the first line of defense against PD. Even if you haven’t accepted your diagnosis, support groups provide the opportunity to learn and share best practices with others who are also battling the condition. The second step is exercise—which is the only therapy scientifically proven to slow down or even delay the progression of Parkinson’s. While there are many theories on what type of exercise is best, my advice as a personal trainer is to find the exercise you enjoy most so that you will do it every day.”
‘Why me?’
Who gets PD and why remains unknown, however, the risk of developing PD is higher for individuals with a family history of the disease, those exposed to certain environmental toxins and those with specific genetic mutations.
“Unfortunately, the science has not determined yet exactly what causes Parkinson’s aside from genetics and has not developed a cure, either,” says Glen. “There isn’t any confirmed information on PD prevention. Some thought has been given to getting regular exercise and eating a well-balanced diet, especially the Mediterranean diet, which has been linked to lower rates of PD. There’s also thought about limiting exposure to environmental toxins like pesticides, herbicides and air pollution to prevent PD.”
According to michaeljfox.org, in most cases, the cause of PD is unknown. “Better understanding of the complex genetic, environmental, aging and other factors that lead to Parkinson’s would be game-changing in our pursuit of preventive and therapeutic treatment options,” the site says.
However, the site goes on to detail possible factors. Although for most people, the cause of PD is unknown (idiopathic), researchers believe that PD is caused by a combination of factors.
With genetic causes at one end and environmental causes at the other, people with PD fall at many different points along the continuum, with some cases due more to genetics, while others are more influenced by environmental factors.
“Scientists are working hard to understand the triggers and the cascade of cellular changes that lead to Parkinson’s. Knowing more about the cause could help researchers develop treatments to stop or even prevent the disease.”
■ Genetics: About 30% of PD risk is explained by genetics. Less than 10% of this risk has been explained by known genetic links, so more PD genes have yet to be discovered. A handful of causal PD genes have been identified in the past 10 years, where genetic mutations greatly increase risk. But not everyone who carries these mutations will get PD, so other factors must play a role.
■ Environment: Head injury and exposure to pesticides have also been identified as factors. Several studies have linked smoking and caffeine consumption to lower rates of PD. “While we do not recommend smoking to prevent PD, understanding these connections can help guide research into the mechanisms and treatment…,” the MFF site says.
■ Aging: Age is the greatest risk factor because our cells may be more susceptible to damage as they age. Researchers project the number of people with PD will double by 2040. In addition, the expression of our genes may change over time, which could set off a chain of cellular events that lead to PD.
■ Combination of Factors: Genetics, environment and aging interact to cause disease. Not everyone with a genetic mutation linked to PD will develop the disease. Similarly, not everyone exposed to a pesticide will be diagnosed. Research into these different triggers continues aggressively every day, including biological/cellular changes.
Hope for the Future
There is significant hope for the future for people with neurodegenerative conditions such as PD. Research is advancing on several fronts. And although there is no simple solution in dealing with a life-changing PD diagnosis, the good news is that most people find acceptance and quality of life after an initial adjustment period.
“I’m more aware of the future now,” says Glen. “Previously, I lived in the moment, thinking only about the present. Now, I think about the future and how my actions now will impact my future. For instance, my personal goal is to never use a mobility device. To accomplish this, I need to consistently exercise and take care of my body and mind. I am living my best life with Parkinson’s by adhering to these simple rules: 1) Be on the right medication plan, which means being open and upfront with my neurologist. 2) You need to exercise. The best exercise is one that you enjoy and will do daily. 3) Finally, having a positive attitude is everything, but if you don’t feel good mentally and physically, it’s hard to have a positive attitude. That’s why being on the right medication plan and daily exercise is so important.”
Glen is a certified fitness professional, working with patients with Parkinson’s as a way to help others live their best lives. He offers Make It Happen Personal Training.
Contact Glen at
808-348-2767, makeithappen@glenhiga.com or
parkinsonshawaii.org/exercise-classes.
For an in-depth guide to navigating PD and living well as the disease progresses, check out the Michael Fox Foundation’s Parkinson’s 360 toolkit at michaeljfox.org/parkinsons-360.
COMMON SYMPTOMS OF PD
Tremors, bradykinesia (slow movements), muscle rigidity and a history of falling or losing your balance are among the most common symptoms. According to the Michael J. Fox Foundation, PD symptoms are different for different people and are difficult for even doctors to detect. Others are obvious, even to an untrained eye.
Motor Symptoms
Motor or movement symptoms seen “from the outside” are used by doctors to make a diagnosis. The three “cardinal” motor symptoms are:
1) Muscle stiffness: rigidity
2) Bradykinesia: a decrease in spontaneous and voluntary movement, such as slower walking, less arm swinging while walking, or decreased blinking or facial expression
3) Resting tremor: a rhythmic, involuntary shaking that occurs in a finger, hand or limb when it’s relaxed, but not during voluntary movement
Not everyone with PD experiences all three motor symptoms, but slowness always is present. And although tremor is the most common symptom, not everyone with PD experiences tremor.
Other Motor Symptoms
Walking, balance and coordination problems may occur any time in the course of PD, but are more likely as the disease advances.
Non-Motor Symptoms
Non-movement symptoms are invisible. You can’t see them from the outside. These common symptoms can affect almost every body system, occur any time in the course of disease (even before motor symptoms or diagnosis) and differ in severity per individual. Non-movement symptoms can significantly impact quality of life:
Autonomic dysfunction: PD can affect the automatic/involuntary functions that our bodies perform: constipation, low blood pressure, sexual problems, sweating problems and urine problems.
Mood and cognitive changes: PD can impact how you feel and think, causing apathy, memoryor thinking (cognitive) problems, mood disturbances, and hallucinations and delusions.
Other physical changes: PD can cause drooling, excessive daytime sleepiness or fatigue, pain, skin changes, sleep problems, smell loss, speech problems, swallowing problems, vision changes and weight changes.
The Fox website (michaeljfox.org) recommends visiting a movement disorder specialist if you think you’re experiencing PD symptoms. Talk to your doctor, especially if what you are experiencing is interfering with activities you want or need to do.
For example, slowness of movement might make exercise more challenging or fatigue might make your workday less productive. Keep in mind that even if you have symptoms common among people with PD, they may be brought on by a completely different condition altogether.
HOPE THROUGH SCIENCE
Advanced & Emerging Treatments
There is hope for people with neurodegenerative conditions such as PD and Alzheimer’s disease (AD), the most common form of dementia. Research is advancing on several fronts:
Deep Brain Stimulation: DBS has long been used for movement problems associated with PD. Newer advancements, such as adaptive DBS, adjust electrical pulses in real-time based on brain signals, providing personalized and potentially more effective symptom control, including non-motor symptoms like mood and sleep dysfunction.
Stem cell therapies: Aim to repair or replace damaged brain cells in PD and AD, with therapies showing promise in clinical trials.
Gene therapies: Reprogram cells to stay healthy and function better, with therapies like AB-1005 (for PD) focusing on stimulating growth factors to minimize dopamine loss.
Drug repurposing: Medications for other conditions, like epilepsy and diabetes, are being investigated for potential AD and PD treatment.
Early Detection & Diagnosis
Biomarkers: Advancements in identifying biomarkers for both PD and AD allow for earlier and more accurate diagnoses.
Advanced imaging: PET scans and other imaging techniques are crucial for visualizing amyloid and tau deposits in the brain, aiding in both diagnosis and treatment monitoring.
AI predictive models: New AI models can forecast brain aging, helping to identify subtle changes indicative of early neurodegenerative disease onset years before conventional methods.
Disease Understanding & Prevention
Genetic factors: Research into genetic variations helps identify individuals at higher risk and explore potential prevention and treatment strategies.
Lifestyle interventions: Studies on lifestyle factors like exercise, diet (e.g., MIND and Mediterranean diets), and management of chronic conditions reveal potential to delay or prevent symptoms.
Improved Care & Support
Personalized medicine: Tailoring treatments based on an individual’s genetic profile and biomarkers holds promise for improving outcomes and minimizing side effects.
Caregiver support: Research focuses on developing strategies to support caregivers and improve the quality of life for those with dementia. While significant challenges remain, particularly in halting disease progression, these developments, ongoing research, advanced diagnostic tools and emerging treatments hold promise for better care, improved quality of life and potentially slowing the diseases’ advancement for individuals living with PD and AD.
This information was extracted and summarized from three 2025 research articles: “This New Treatment Can Adjust to Parkinson’s Symptoms in Real Time,” “Research on Alzheimer’s Disease and Related Dementias” and “Advancements in the treatment of Alzheimer’s disease: a comprehensive review.”
The Power is Yours
The Hawai‘i Parkinson Association (HPA) is a nonprofit, all-volunteer group comprised of people living with Parkinson’s disease (PD), caregivers, family members, healthcare professionals, educators and leaders in the business community. You, too, can become part of the solution through your volunteerism and/or donations. Donations directly benefit those living with PD and their caregivers in our island community.
VOLUNTEER
Go to parkinsonshawaii.org/get-involved and fill out a form to indicate your volunteer interests.
DONATE
As an independent nonprofit, all funds raised in Hawai‘i stay in Hawai‘i. Donations are accepted online at parkinsonshawaii.org/donate or donate by mail. Checks are payable to Hawai’i Parkinson Association and can be mailed to the address below. Donations are fully tax-deductible. Hawai‘i Parkinson Association Resource Center 2228 Liliha St., Ste. 206 | Honolulu, HI 96817
HPA RESOURCE CENTER
The HPA Resource Center is available to everyone in the community looking for information about Parkinson’s disease. HPA has information on doctors, clinical trials and support groups on O‘ahu, the Big Island, Maui and Kaua‘i.
Medical specialists: parkinsonshawaii.org/medical-specialists
Local clinical trials: hawaiineuroscience.com, 808-261-4476
Online and in-person seminars: Experts offer information on many different topics. If you have a topic you’d like to suggest, contact HPA.
Peer-to-peer connect: Whether you’re newly diagnosed, have had PD for a while, or are a caregiver or family member, HPA can connect you via phone or email to one of its volunteers.
Support groups: parkinsonshawaii.org/support-groups: Support groups are a great way to make connections with other people with PD and their caregivers/partners and share experiences on living well with Parkinson’s.
Books, brochures & flyers are available from various PD organizations with information about symptom management, medical and complementary therapies, and adaptive equipment.
Lending library: The center houses a growing library of books to borrow at no cost. Stop by or contact HPA for a list of available books. Reserve a book for pickup or donate a book that you’d like to share with others.
Exercise classes: parkinsonshawaii.org/exercise-classes: Exercising is a very important part of managing PD. HPA can give you information about the people and places who can modify their classes for PD. From yoga to boxing, there is something available for you.
Assistive technology:
– Soderholm Mobility: soderholmmobility.com, denise@soderholmbus.com, 808-834-1417
– Assistive Technology Resource Centers of Hawaii: atrc.org, 808 -532-7112
– Complementary therapies: parkinsonshawaii.org/complementary-therapies
HAWAI‘I PARKINSON ASSOCIATION (nonprofit)
Glen M. Higa, President
808-348-2767 | president@parkinsonshawaii.org
Resource Center:
808-762-0600 | info@parkinsonshawaii.org
parkinsonshawaii.org
The medical information contained in this article is for general information purposes only. The Michael J. Fox Foundation for Parkinson’s Research has a policy of refraining from advocating, endorsing or promoting any drug therapy, course of treatment, or specific company or institution. It is crucial that care and treatment decisions related to Parkinson’s disease and any other medical condition be made in consultation with a physician or other qualified medical professional.




Leave a Reply