We are compassionate people who avoid pain and go to great lengths to protect our loved ones from suffering. So why is there controversy about Hawai‘i’s Our Care, Our Choice Act, the aid-in-dying law that allows terminal patients to have medications that will ensure a peaceful passing?
One night sticks in my memory. Mild-mannered Pete had an aggressive brain tumor that slowly paralyzed him; no therapy would cure it. His wife, Carole, was a genius at finding ways to overcome his growing disabilities — taking him out for lunch,
to concerts or playing with the grandkids. Pete never experienced the crushing pain I saw with patients on chemotherapy.
 One evening, Carole called and told me Pete’s breathing sounded like gurgling. I rushed to the house to help; I knew the end was near.
One evening, Carole called and told me Pete’s breathing sounded like gurgling. I rushed to the house to help; I knew the end was near.
It’s impossible to know what to do or say, but being with loved ones seems to help. Hospice was at the house to ensure Pete was not experiencing pain. His frail chest rose and fell at a rapid pace as he struggled for air for over an hour. Our priest came in and performed the last rites. Pete kept hanging on.
The family could do nothing but watch him struggle. Even in his delirium, Pete was fighting death to the end. Hospice gave him more morphine and finally the death throes stopped — the first silence in many hours. Tears gave way to funeral preparations and paperwork. Eventually, Carole and the kids’ memories healed; consolation came.
I don’t have children and won’t be able to afford skilled nursing, so I plan to die at home. Last year, arguments for “dignity in dying” and others against “assisted suicide” honestly confused me.
Quality of life is my focus. I am in my 70s, and over the summer, I injured my back and couldn’t walk. Physical therapy cured my back, but being disabled for a while made me seriously consider how I would handle being dependent on others for daily care. Will I choose to fight a terminal disease to the last breath like Pete? Not a chance; I am a lover, not a fighter. I’d really like to die in my sleep, peacefully, like my mom did. Can I do that?
What “Choice” Are We Talking About?
Getting at the facts about our Hawai‘i law…
“Compassionate Choice,” “Medical Assisted Death,” “Assisted Suicide” and “Dignity in Dying” are ways people refer to aid-in-dying laws in many states that allow terminal patients to avoid suffering when they die. The various names reflect deeply held feelings people may have about death, dying or end-of-life. Even between friends, the taboo topic is oven avoided, because bringing it up unleashes our worst fears and saddest memories.
Generations Magazine believes that our readers can only plan for the future and live well if they have all the facts. Smart seniors manage to live independently, enjoy life and prepare themselves for the future, whatever it brings. Akamai seniors also need to consider their options based on Hawai‘i’s recently enacted aid-in-dying law.
So we found people with the most information about Hawai‘i’s Our Care, Our Choice Act (OCOCA), which has been in effect since Jan. 1, 2019. You can decide the pluses and minuses, understand the knowns and unknowns, and read the facts about how the law is working after its first year in practice.
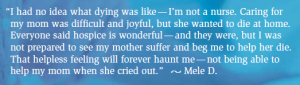
Let’s start with an interview with the daughter of a terminally ill woman who used medical aid-in-dying via the OCOCA last year. Kim McAden was very sad to lose her mom, but was glad to be able to honor her mother’s decision to stop prolonging her suffering once there were no more options for a cure.

The Passing of Jeanne Elder,
Easter Sunday, 2019
An interview with her daughter, Kim McAden
“My mother, Jeanne Elder, always had this in her mind since the 1970s. She did not want to be disabled by a terminal disease. I think she didn’t want to be trapped and unable to make her own decisions — particularly if there was no hope for recovery.
“When my mom was diagnosed with melanoma three years ago, the disease had already escaped the lymph nodes. She went through immunotherapy on O‘ahu and in San Diego. The side effects she suffered were very troubling for her and for us.
“In January 2019, she had pain in one arm and found the disease had metastasized to her spinal cord. By the end of February, the cancer progressed and she could walk no longer, but she was not ready to quit. ‘I will still fight,’” she said.
“By April, Mom felt she had lost her battle with cancer. She didn’t want to leave us, but with melanoma winning, she decided to participate in the Our Care, Our Choice law enacted January 2019. I remember what she said: ‘This needs to happen. I am a resident of Hawai‘i and this is my decision. It’s the law; they have to let me do this.It is my decision.’
“As her caregiver, I encountered many problems carrying out her wishes under the new law. I was her advocate and my e experience as a purchasing manager for biotech companies gave me the sourcing skills I needed to help her, but everyone in this situation may not have these skills.
“The Social Worker Association of Hawai‘i was outstanding — they admitted that my mom was their first patient seeking a psychological evaluation for an OCOCA prescription. They offered to put out feelers to their members on Facebook and by email. The in-home psychological evaluation they lined up helped qualify Mom for OCOCA and I cannot emphasize enough what a kindness this assistance was to our family.
“Mom’s attending oncologist also faced uncharted territory with my mother’s case. After much soul searching, he worked with his staff to create new policies and protocols concerning medical aid-in-dying. When they were in place, he visited my mother at Hospice Hawaii for a final evaluation. It was comforting to know we had his support. We will be eternally grateful for his love and care.
“Jeanne Elder was a charming, adventurous, passionate, beautiful, independent woman. She fought against the stereotypes beautiful woman face and enjoyed great respect. She owned a successful business and a beautiful home; she took great joy in traveling the world.
“I wish everyone could understand how peaceful my mom’s passing was. She never lost her dignity. In her bedroom were family, friends, flowers and music. She passed in 30 to 45 minutes. She fell asleep in about 10 minutes and had just a little labored breathing, but her death was very peaceful and beautiful. I feel like she’s a part of all of us now.
“For readers who are family caregivers and advocates, I encourage them to honor and respect their loved one’s wishes. Be strong, take one step at a time and don’t get overwhelmed. Download all the information you can, ask questions and expect things to change every day. If the pressure gets too great, it’s okay to back out or take a rest — but do try to find someone to take your place. I think this goes for all family members and attending medical staff. There are lots of support resources for you — you are not alone. May your path forward be filled with peace and love, knowing your loved one’s wishes were honored.”

Is Our Care, Our Choice About Avoiding Pain?
Pain is not what I am worried about…
Our first inclination is to think of medically assisted death as a way to avoid pain. But in fact, doctors today have many medications to treat pain. The main service hospice provides is “palliative care,” which does not necessarily treat the condition, but keeps the patient comfortable and controls pain.
Nevertheless, hospice professionals point out that terminal patients suffer two more things — the debilitating outcomes of their disease and the effects of the curative therapies they undergo, such as surgery, chemotherapy or radiation. Convulsions, incontinence, tremors, hallucinations, disabilities and increasing dependency can rob patients’ dignity. Doctors and hospice nurses will try to modify these problems, but what the patient might consider good quality of life may not return.
Some patients will resign themselves to decline and embrace death. Others deny the inevitable and fight for every last breath. Until last year, a terminal patient’s only options were to discontinue medications and efforts to keep them alive on machines. And the only way they could hasten their death was to refuse water and food.
OCOCA Patient Zero Advises,
“Plan Your Peace”
An interview with John Radcliffe, former lobbyist and business owner…
The first terminal patient in Hawai‘i to request a prescription for OCOCA medications to induce sleep and death is still living and able to give us guidance! I call him “Patient Zero.” John Radcliffe was diagnosed with terminal stage 4 cancer in June 2014. When he heard that an aid-in-dying bill was proposed at the Hawai‘i Legislature, he stepped out of retirement to exercise one of his talents — lobbying. John’s passion for the right to legally choose how and when he would die ran deep. He wanted to help extend that choice to everyone while fighting his own terminal cancer. His advice to patients facing death is to take action and plan your end-of-life while you can.
“I had ‘inoperable cancer’ and they gave me six months to live,” says John. “No law would allow me to choose a peaceful death if my suffering got to be too intense. If I wanted to die at home, there was no way to protect my loved ones from watching me struggle and suffer at the end.

“Chemotherapy was rough, but when I felt good enough, I helped push the various aid-in-dying bills in the Hawai‘i’s House of Representatives and Senate. And what do you know? When the law passed, I was still alive — after over 80 rounds of chemo! So I was the first terminal patient in the state to begin the process of getting a prescription for the peaceful death cocktail of medications.”
John is very clear in his advice to newly diagnosed terminal patients with six months or less left to live.
“Don’t delay! If you believe your diagnosis, get your affairs in order and plan how you want to spend your last days — how, where and with whom you want to die,” he says. “Cancer is unique for every patient — it goes wherever it wants in your body. It’s going to destroy you and nobody can give you advice (but they will try!). Friends insisted I take every herb, root, berry and leaf. But we have excellent healthcare in Hawai‘i, so if you trust your doctors, do what they tell you.
“It is most important to free yourself of stress and pressure. You don’t know how much time you really have to find a little peace and happiness for your end-of-life. People don’t think about what really counts and how they will die until it’s upon them. I was fortunate to outlive my first prognosis, but I am pretty content now. If things get rough, I have the confidence of knowing that a peaceful death is within my control. I’m not ready today, but I will know the time,” he says.
John was a teacher in Chicago before he moved to O‘ahu in 1980. A lobbyist and small business owner, he was the perfect terminal patient to “test the waters” and determine if the law would work for the first patient. He already knew Dr. Chuck Miller, former head of hematology and oncology at Kaiser Permanente, and now working part-time in his retirement as an aid-in-dying specialist for Kaiser. Dr. Miller helped advocate for OCOCA by providing our legislature medical data and testimony based on his decades of clinical experience with thousands of terminal cancer patients.
But after John qualified for OCOCA and Dr. Miller prescribed the approved medications, it took John 60 days to get his prescription filled! By law, the drugs must be formulated by a pharmacist licensed by the State of Hawai‘i to “compound” or mix up the specific combination of medications. Fortunately, ElixrRx in Kailua meets all the state standards.
When John eventually does choose to use his medications, he will have to take an anti-nausea pill 45 minutes before he drinks the drugs. The powders come in separate vials, so he, a nurse or family member will mix them together and add water. Then, John must drink the medication cocktail himself. A nurse or loved one may help him hold the cup or put a straw in the cup, but he will “administer” the drugs to himself. That’s how the law works.
In the last four, going on five “bonus” years of John Radcliffe’s life, he has connected with family and enjoyed some of the retirement for which he worked so hard. “A son I never knew I had searched me out. He brought my grandchildren and great grandbabies to visit me! They are a wonderful family, and getting to know them (they all look like me) has brought unspeakable joy,” says John. He says substituting stress with joy has helped him develop a profound sense of gratitude for every day.
“And in a way, my life is really better than it has ever been,” he says.
John expresses the contentment medical aid-in-dying can bring to terminally ill patients while they are still living. In Oregon and Washington, a quarter of the patients who receive prescriptions for the medications don’t take them. Just knowing that they have options is enough. So, John Radcliffe’s advice to “plan your peace” is solid.
Medical Aid-in-Dying is Old News
Where can I find the official facts for Hawai‘i residents?
Medical aid-in-dying is now legal in nine states. For 25 years, Oregon citizens have been able to self-administer medications to hasten death. In 1992, Gov. Ben Cayetano’s Blue Ribbon Committee proposed a Hawai‘i Death with Dignity law, but it was defeated by the slimmest of margins. By 2017, support among Hawai‘i registered voters for Our Care, Our Choice was close to 80 percent. Still, the bill was tabled until the 2018 legislative session, when it passed by a wide margin.
In April 2018, Gov. David Ige signed the Our Care, Our Choice Act. As previously mentioned, the law went into effect just over a year ago. National nonprofit Compassion & Choices, with decades of experience in Oregon and many other states, provided essential data and patient experiences for Hawai‘i legislators to consider. Our law resembles Oregon’s but has added patient safety provisions that reflect our more conservative culture. (CLICK HERE here for online resources.)
Dr. Charles Miller, MD, Director of the Aid-in-Dying Program, Kaiser Permanente
Dignity, autonomy, control over my options at my end-of-life — now that interests me…
 Chuck Miller, MD, began volunteering with Compassion & Choices in 2002. He came to Honolulu in 1999, was head of hematology and oncology at Tripler Army Medical Center, and chief of hematology-oncology at Kaiser Permanente. After retiring, he supported Hawai‘i’s OCOCA legislation and now practices part-time at Kaiser Permanente to help administer the aid-in-dying program for terminally ill patients. He explains that his medical opinions are not necessarily the policies of Kaiser, because he is still researching ways to improve OCOCA procedures.
Chuck Miller, MD, began volunteering with Compassion & Choices in 2002. He came to Honolulu in 1999, was head of hematology and oncology at Tripler Army Medical Center, and chief of hematology-oncology at Kaiser Permanente. After retiring, he supported Hawai‘i’s OCOCA legislation and now practices part-time at Kaiser Permanente to help administer the aid-in-dying program for terminally ill patients. He explains that his medical opinions are not necessarily the policies of Kaiser, because he is still researching ways to improve OCOCA procedures.
“I am very impressed with Kaiser and its integrated healthcare system that delivers good palliative care to terminal patients. Every patient is unique, and Kaiser brings together all the medical, social and coordinated hospice support needed for each patient’s individualized journey.
“People always ask me why people would choose medical aid-in-dying if they’re going to die anyway. Intuitively, we guess it is a move to avoid pain, but doctors have great options for managing pain. Hospice is all about managing pain for terminal patients.
“What I observe is that medical aid in dying gives people back the control that they lose to their disease. Overwhelming disease and complicated treatments rob their identity, self-worth and autonomy. Terminal disease is the tail wagging the dog, which is the patient family and care team. So, planning out how, when, where and with whom you will die has the effect of restoring autonomy and a sense of control and self-esteem.
“Experience from 22 years of legal medical aid in dying in Oregon shows us that some patients who ask for the medication don’t take it. We see the same thing in Hawai‘i. This year, a total of 44 Kaiser patients made requests for medical aid in dying; 42 were deemed eligible by the state DOH. Of those, 21 patients received prescriptions and 10 self administered the medications. Another 15 died of their diseases without taking the medication. Still, all had options and felt in control.

“The patients I feel bad about are the ones who want the OCOCA option but don’t survive the 20-day waiting period. I can tell at that first evaluation meeting whether the patient is going to live for three weeks. This year, six of my terminal patients died too soon to meet state requirements. I encourage terminally ill patients to plan end of life options as soon as they know they have six months or less to live. Don’t wait. See if your family doctor will support you through end-of-life.
“The good news is that the Hawai‘i law is working as intended. OCOCA patients experienced peaceful deaths, and there were no incidents of coercion, abuse or medications falling into the wrong hands. Kaiser follows up with OCOCA families and all expressed satisfaction that the patient received the treatment they wanted.
“It’s so important that family caregivers seek hospice care as loved ones near end-of-life. Hospice services help both patient and family before, and immediately following death. Besides administering pain medications, they interact with the doctor who pronounces time of death, help fill out records and call the mortuary to collect the body. For the sake of your family, engage hospice for terminal patients.
“If we all tell a friend about what we learned about OCOCA this year, we can offer many more terminal patients this important option.”
Aid-in-Dying Prescriptions:
Pharm D Jake Blechta
ElixRx Pharmacy, Kailua
So, what will self-administering the aid-in-dying medication really be like?
After a patient’s request to qualify for medical aid in dying is approved by DOH, his or her doctor prescribes medications that induce sleep and s peaceful death.
Jake Blechta, Pharm D, owns ElixRx, an independent specialty pharmacy on O‘ahu. In 2019, Blechta filled the most aid-in-dying prescriptions in the state. He is specially licensed to “compound” the prescription for each individual patient, according to legal guidelines.
“I counsel all my patients how to take their prescriptions, but Kaiser treatment teams have already reviewed drug affects and how to self-administer, so families do not have many questions.
“OCOCA-qualified patients receive two different anti-nausea pills to take one hour before they plan to drink the main drug. After an hour, they or their caregiver mix the powdered drug compound into six ounces of liquid. They may use any non-dairy beverage the patient is used to drinking — water, juice or even a cocktail — and mix it very well. The resulting liquid is pretty thick and the patient must drink it right down, because I don’t think it tastes very good.
“Patients can expect to fall asleep quickly, within the first hour, and then pass peacefully in their sleep within four hours. It appears that some patients get the drugs for reassurance and end up not needing to take them,” says Blechta.
• • •
So there we have it. Death and dying will always challenge us. For some, it is a matter of faith; others want to make sense out of our lives, say goodbyes or make amends. Getting our affairs in order takes many forms.
Plantation values teach us to prepare for the worst; hope for the best. The days usually roll out somewhere in the middle of what we can handle. If you have loved ones who are terminally ill, support their choices with joy. If you are nearing the end of your life and need help to get your ducks in a row, be sure to share your plans with your loved ones, family and medical team. You may need some assistance choosing your peace.
Terminal Patients Must Meet the Following DOH Requirements:
• Hawai‘i state resident 18 years of age or older
• Diagnosed terminal illness with six months or less to live
• Able to self-administer the aid-in-dying medication
• Make two oral requests not less than 20 days apart to your Hawai‘i-licensed attending physician
• Mentally capable of making a voluntary, informed decision (without coercion)
• Able to complete one written request and declaration signed by two independent witnesses and written in a specific format
• Meet the OCOCA criteria with a consulting attending physician and a mental health counselorOnline Resources
– DOH: The Our Care, Our Choice Act www.tinyurl.com/DOH-OCOCAInfo
– DOH Written Request Form www.tinyurl.com/DOHWrittenReqForm
– DOH Attestation Form www.tinyurl.com/DOHAttestationForm (Medicare can pay for the medication but only from Hawai‘i state funding.)
– SHIP Hawaii: 808-586-7299 on O‘ahu, 888-875-9229 on neighbor islands
– Compassion & Choices Hawaii Resources www.compassionandchoices.org
– Kōkua Mau Resources www.kokuamau.org
By Katherine Kama‘ema‘e Smith
Photography by Brian Suda



Leave a Reply